Background
A hallmark characteristic in patients with Sickle Cell Disease (SCD) is chronic hemolysis, the severe exacerbation of which has been linked to RBC transfusion in some cases. This hyper-hemolysis (HH) is defined as a rapid decline of hemoglobin (Hb) and HbA% below pre-transfusion values. HH has been considered a severe form of antibody negative DHTR (Ab (-) DHTR) in patients with SCD and defined by the American Society of Hematology as hemolysis within 21 days of transfusion, negative DAT and absence of new alloantibody. Herein, we present a case series of 5 SCD patients with transfusion > 21 days from presentation demonstrating symptoms and lab findings consistent with HH. The purpose of this study is to characterize patients with SCD diagnosed with HH as a working diagnosis without temporal relation to transfusion. To our knowledge, this is the first and largest case series of its kind.
Methods
An IRB approved retrospective EMR review collected demographic and clinical data for patients with SCD admitted for concern for HH or DHTR to a large multi-site Pediatric Hospital in the Southeastern USA (2020-2023). All patients in this study were identified from Transfusion Medicine consults to investigate DHTR. Patient admission diagnosis was obtained from EMR review.
Findings
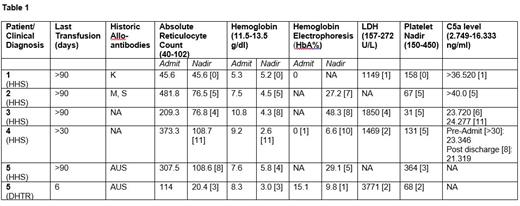
Cohort patients were 15-19 years with HbSS or HbS-beta thalassemia zero. All patients had transfusion >21 days from presentation. Of note, patient #5 received a transfusion during their first admission and was readmitted for signs and symptoms of HH/Ab (-) DHTR within 24hrs of discharge. All patients admitted for >1 day demonstrated an average 47% fall in hemoglobin (range: 24-69%), negative antibody screen/DAT, reticulocytopenia and mild to moderate thrombocytopenia. Four patients demonstrated elevated LDH. One patient died prior to discharge. Day of stay (DOS) of labs is in brackets []. Refer to table 1 for detailed patient data.
Conclusion
This case series demonstrates that patients with SCD can experience a constellation of symptoms identified in patients with HH without temporal relation to transfusion. These include hemolysis, reticulocytopenia, and thrombocytopenia as well as elevation of complement proteins. Given the overlap in presentation, HH in patients with SCD should be considered independently of proximity to transfusion for prompt diagnosis. Further study should include a retrospective review for further characterization. In addition, given the finding of elevations in C5a, further study into complement as a mechanism and target of therapy would be valuable.
Disclosures
Chonat:Roche/Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda Pharmaceuticals: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; GBT/Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Alexion: Consultancy, Other, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal